Understanding the Alzheimer’s Disease Assessment Scale Cognitive (ADAS-Cog): A Comprehensive Guide
The Alzheimer’s Disease Assessment Scale Cognitive (ADAS-Cog) is a widely recognized and utilized tool in the field of neurology and geriatrics. Designed to evaluate cognitive function in individuals with Alzheimer’s disease and other forms of dementia, the ADAS-Cog provides a detailed assessment of various cognitive domains. In this article, we will delve into the intricacies of the ADAS-Cog, exploring its origins, structure, administration, scoring, and clinical implications.
Origins and Development
The ADAS-Cog was developed in the early 1980s by a team of researchers led by Dr. John C. Morris. The scale was created to address the need for a standardized, comprehensive assessment of cognitive function in patients with Alzheimer’s disease. Initially, the scale was designed to be used in clinical trials, but its utility has expanded to include diagnostic and prognostic purposes in clinical practice.
Structure of the ADAS-Cog
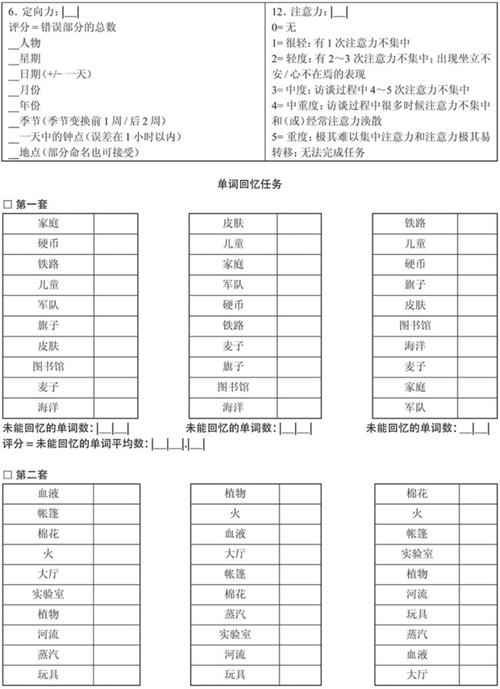
The ADAS-Cog consists of 11 individual tests that assess various cognitive domains, including memory, language, and praxis. These tests are categorized into three main sections: memory, language, and orientation. The memory section includes tests for immediate and delayed recall, while the language section evaluates naming, repetition, and comprehension. The orientation section assesses the patient’s ability to identify time, place, and person.
Administration of the ADAS-Cog
The ADAS-Cog is typically administered by a trained healthcare professional, such as a neurologist or geriatrician. The assessment takes approximately 30 minutes to complete and involves a series of tasks and questions designed to evaluate the patient’s cognitive abilities. The tests are performed in a quiet, well-lit room, and the patient is seated in a comfortable chair. The examiner reads instructions and asks questions, while the patient responds accordingly.
Scoring the ADAS-Cog
The ADAS-Cog uses a standardized scoring system to quantify the patient’s cognitive performance. Each test is scored on a scale of 0 to 10, with higher scores indicating worse cognitive function. The total score is calculated by summing the scores of all 11 tests. The raw score can then be converted to a standardized score, which allows for comparison with normative data and other patients.
Table 1: ADAS-Cog Test Scores and Interpretation
| Test Score | Interpretation |
|---|---|
| 0-10 | Severe cognitive impairment |
| 11-20 | Moderate cognitive impairment |
| 21-30 | Mild cognitive impairment |
| 31-40 | Normal cognitive function |
Clinical Implications of the ADAS-Cog
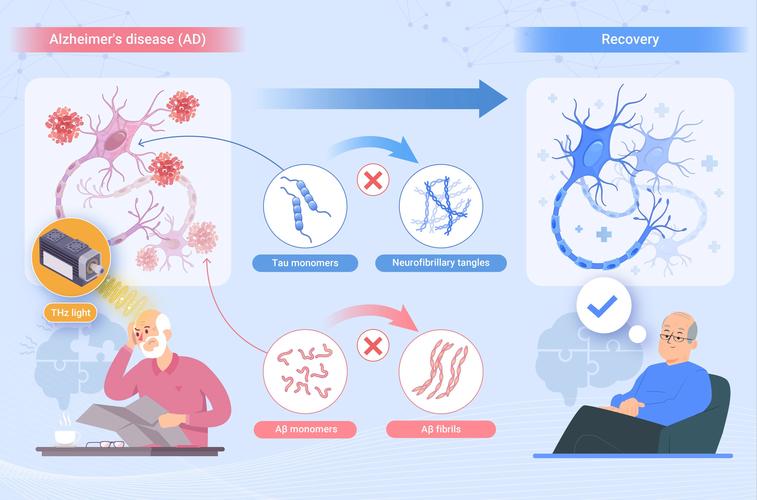
The ADAS-Cog has several clinical implications, including diagnosis, treatment planning, and monitoring disease progression. As a diagnostic tool, the ADAS-Cog can help healthcare professionals differentiate between Alzheimer’s disease and other forms of dementia. It can also be used to monitor the effectiveness of treatment interventions and to predict the prognosis of patients with Alzheimer’s disease.
One of the key advantages of the ADAS-Cog is its ability to detect subtle changes in cognitive function over time. This makes it an invaluable tool for researchers and clinicians alike. By tracking the progression of cognitive decline, the ADAS-Cog can help inform treatment decisions and improve the quality of life for patients with Alzheimer’s disease.
Limitations of the ADAS-Cog
While the ADAS-Cog is a valuable tool, it is not without limitations. One of the primary limitations is its reliance on self-reported information from the patient and their caregivers. This can introduce bias and inaccuracies, particularly in patients with severe cognitive impairment. Additionally, the ADAS-Cog may not be sensitive enough to detect changes in cognitive function in the early stages of Alzheimer’s disease.
Conclusion
The Alzheimer’s Disease Assessment Scale Cognitive (ADAS-Cog) is a comprehensive and widely used tool for evaluating cognitive function in patients with Alzheimer’s disease and other forms of dementia. Its origins, structure, administration, scoring, and clinical implications make it an invaluable resource for healthcare professionals



